Decades ago, the first picture parents saw of their baby might have been just a blurry black-and-white outline; today, they might receive a real-time, dynamic 4D image, even seeing facial features outlined by AI. Where did this change come from? Is it that doctors have changed, or that the machines have "evolved"? The answer is undoubtedly the latter.
So, from those initial black-and-white images to today's AI-assisted diagnostics, what exactly has changed about ultrasound machines? To understand this, we first need to go back to the beginning.
![From Black and White to AI What’s Changed in Ultrasound Machines From Black and White to AI What’s Changed in Ultrasound Machines]()
What is an Ultrasound Machine and How Did It Begin?
An ultrasound machine is a medical imaging device that uses high-frequency sound waves to produce real-time images of the human body's interior. Unlike X-rays or CT scans, it does not use ionizing radiation, making it a very safe and versatile tool for observing soft tissues, organs, blood flow, and developing fetuses.
How it works:
Its core principle is echolocation, similar to the navigation methods used by bats or submarines.
After applying gel to the transducer, it is placed on the skin. The probe emits high-frequency sound pulses into the body. If it encounters a tissue boundary (such as an organ wall, a fluid-filled cyst, or moving blood cells), the pulses will be reflected to the probe at different intensities and speeds. The computer then calculates the distance and intensity data of each echo, constructing and continuously updating a detailed two-dimensional (or even three-dimensional) grayscale image on the screen, allowing doctors to observe tissue structure, movement, and function in real time.
![adoctor is using the early ultrasound machine adoctor is using the early ultrasound machine]()
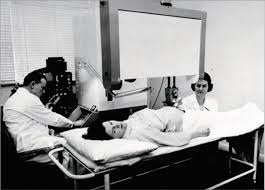
How did it begin:
The development of medical ultrasound is a history of applying wartime technology to the great cause of peace and saving lives.
This journey began with the study of sound and acoustics. Scientists learned echolocation from bats, leading to the development of sonar. After World War II, Scottish obstetrician Ian Donald began using industrial ultrasonic flaw detectors to examine tumors. In 1958, he and his team published a landmark paper demonstrating the enormous diagnostic potential of ultrasound by using it to differentiate between cysts and solid tumors. The earliest ultrasound devices could only generate simple one-dimensional waveforms (A-mode).
In the 1960s and 70s, advances in computer speed and the invention of polycrystalline array transducers led to the first commercially successful real-time ultrasound scanner, allowing doctors to see cross-sectional images of the human body.
From the 1980s to the present, technology has advanced rapidly. The emergence of Doppler ultrasound and 3D/4D ultrasound has revolutionized the use of ultrasound scanners in medical diagnostics. Meanwhile, the size of machines has shrunk from bulky devices to handheld devices that can connect to smartphones. Today, the integration of AI is the latest cutting-edge technology, which helps automate measurements, improve image quality, and assist in the identification of potential anomalies.
What Changed and What Problems Did It Solve?
The evolution of ultrasound equipment is essentially a story of overcoming three major diagnostic challenges. Each leap forward has not only made images clearer, but has also opened up new dimensions for clinical diagnosis.
The Evolution of Grayscale Imaging
Early ultrasound resembled an auditory device, requiring doctors to rely on experience to "interpret" the height and location of waveforms to infer the depth and nature of lesions. It answered the question, "There's an abnormality," but couldn't show "what the abnormality actually looks like."
With the rapid development of computer and probe technology, ultrasound has leaped from "hearing echoes" to "seeing images." The essence of this upgrade is converting echo signals into light spots of varying brightness, then converging them onto the screen to form a complete, real-time updated two-dimensional cross-sectional image. From then on, doctors no longer needed to interpret abstract waveforms; they could directly observe organ structures like anatomical slices.
Breakthrough in Motion and Blood Flow Imaging
While grayscale ultrasound provides clear anatomical images, it ultimately presents a static, "mimetic" picture. Doctors still cannot assess the heart's beating and pumping function; they can detect a tumor, but struggle to identify the blood vessels supplying it.
The breakthrough in the crucial diagnostic dimensions of motion and blood flow lies in the ingenious application of the "Doppler effect." When sound waves encounter a moving object (such as flowing blood cells), their echo frequency changes. By capturing and analyzing this frequency shift, the ultrasound machine can calculate the velocity and direction of blood flow. This technology has brought two key upgrades:
![Breakthrough in Motion and Blood Flow Imaging Breakthrough in Motion and Blood Flow Imaging]()
This breakthrough has made the ultrasound machine a powerful assessment system, opening new doors for precise diagnosis in multiple medical fields, including cardiovascular medicine, obstetrics and fetal medicine, and tumor diagnosis.
The Integration of Intelligence and Automation
With high-definition grayscale images and dynamic blood flow information becoming standard, reliance on experience has become a new bottleneck: From finding standard sections to measuring key data and identifying subtle features, everything depends on the doctor's technique and experience. The entire process is cumbersome, time-consuming, and difficult to standardize completely.
AI and Automation technologies have solved this problem, allowing machines to begin taking on some of the "observation, measurement, and thinking" tasks.
Image Enhancement: Algorithms can optimize image quality in real time, such as automatically suppressing noise and enhancing tissue boundaries, reducing the stringent requirements on the initial image acquisition techniques.
This breakthrough has raised the quality baseline in primary healthcare examinations while improving efficiency.
Future Outlook
Looking back at the evolution of ultrasound from black-and-white outlines to intelligent insights, its core driving force has always been the desire to understand the mysteries of life earlier, more accurately, and more safely.
The future evolution of ultrasound devices will see further miniaturization in form, with even ultra-miniature probes at the level of biosensors potentially emerging. These will be wearable and implantable, enabling long-term, dynamic monitoring of bodily indicators. Functionally, they will evolve from passive assisted diagnosis to active detection and dynamic assessment. What further upgrades can ultrasound achieve in the future? The answer may no longer focus on a single technology, but rather on a fundamental paradigm shift and upgrade.
English
العربية
Français
Русский
Español
Português
Deutsch
italiano
日本語
한국어
Nederlands
Tiếng Việt
ไทย
Polski
Türkçe
ພາສາລາວ
ភាសាខ្មែរ
Bahasa Melayu
ဗမာစာ
Filipino
Bahasa Indonesia
magyar
Română
Čeština
Монгол
қазақ
Српски
हिन्दी
Slovenčina
Slovenščina
Norsk
Svenska
українська
Ελληνικά
Suomi
Հայերեն
עברית
Latine
Dansk
Shqip
বাংলা
Hrvatski
Afrikaans
Gaeilge
Eesti keel
Māori
नेपाली
Oʻzbekcha
Български
ქართული
Кыргызча